Forme Catheter
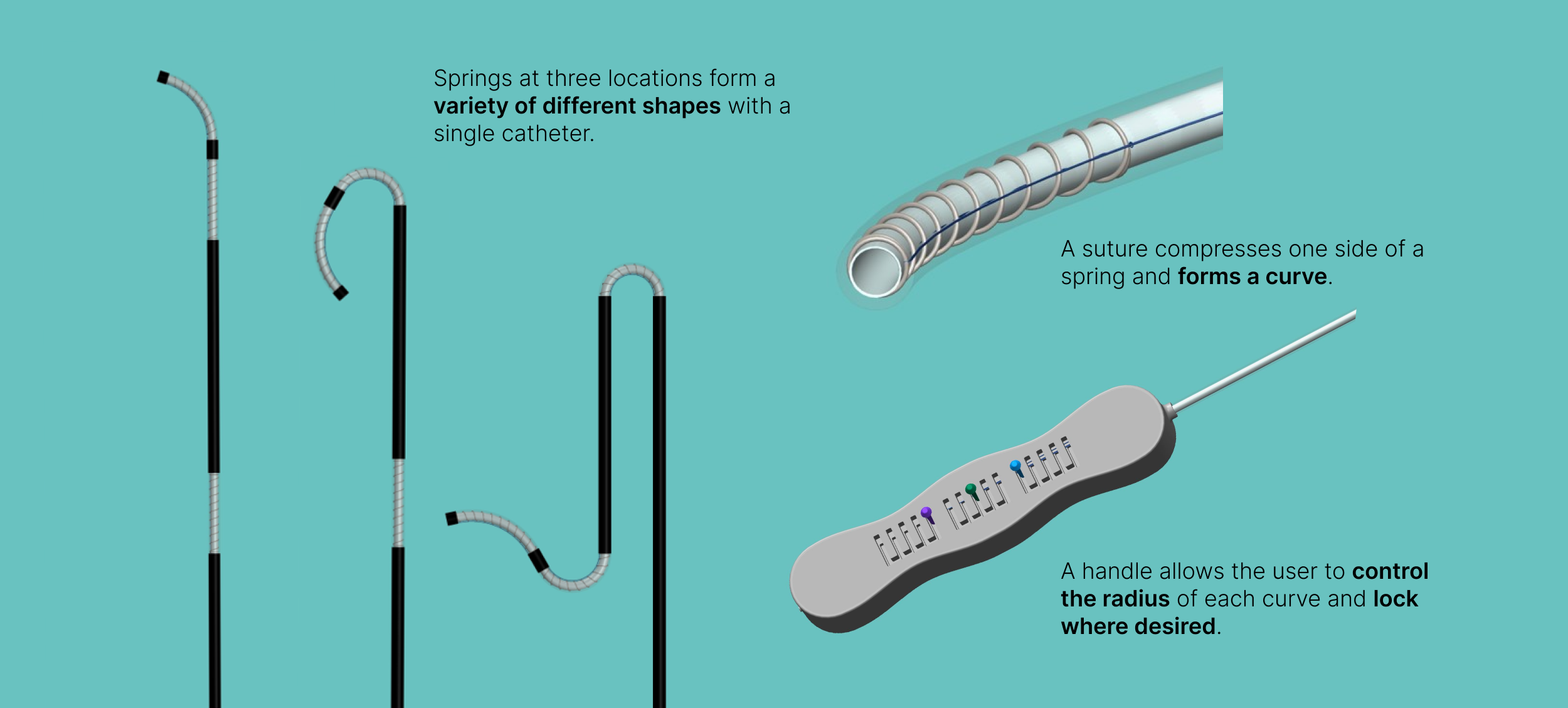
Forme catheter is a novel arterial catheter that can change shape in real-time in response to a patient’s unique vasculature. It contains embedded springs at three different locations that compress to form a variety of different shapes within a single catheter.
Project Introduction
Timeline
January-April 2018
Tools
SolidWorks, 3D printing, Google Suite
Project Type
Biomedical Engineering Undergraduate Capstone Project
My Primary Contributions
User interviews, Fly-on-the-wall observations, Concept ideation, 3D modeling, Design requirements, prototyping, Usability testing
Project Team
Katie Jordan (Research Engineer)
Alexa Schlein (Design Engineer & PM)
Lemou Tieyan (Research Engineer)
Diana Yunda (Design Engineer)
My team designed the Forme Catheter, an adaptive catheter shaping the future of interventional radiology.
As part of a semester-long senior undergraduate capstone course in Biomedical Engineering, I worked with three classmates to design a catheter to resolve issues that occur during interventional radiology procedures. We were mentored by three Interventional Radiologists from Emory University Hospital Midtown in Atlanta, GA. I acted as both project manager and design lead, generating a medium fidelity physical prototype. My team and I won Best Overall Project out of over 200 teams from various engineering disciplines at the Spring 2018 Georgia Tech Capstone Design Expo.
Let’s talk about the problem.
Background
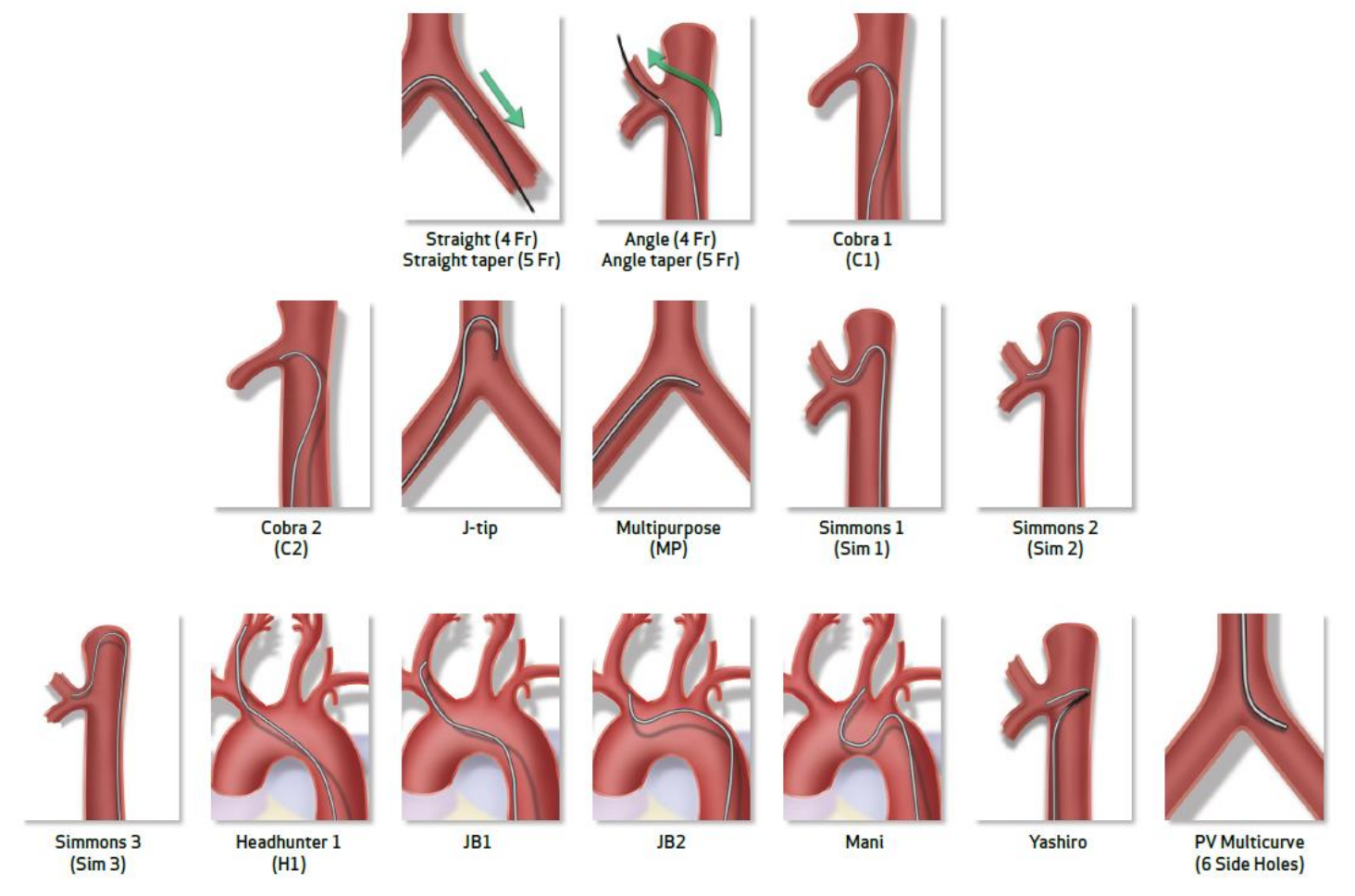
Current catheters routinely placed by interventional radiologists, critical care physicians, vascular surgeons, cardiologists, nephrologists, and other specialists often have singular shapes and functions. A gastrointestinal bleed (GIB) occurs when there is bleeding in the gastrointestinal (GI) tract, which can range from a slow bleed to a life-threatening hemorrhage. In each procedure to treat GIB, an interventional radiologist (IR) uses 3-10 base/diagnostic catheters. Each catheter sells at $15-50 per unit, which can be conservatively estimated to a market of $3.33 million per year. If the patient anatomy changes configuration (such as from occlusion) the catheter may become nonfunctional. In addition, the needs of the patient may change. Currently available on the market are steerable catheters and pre-shaped catheters. Steerable catheters are expensive ($2000 per unit) and IRs do not find their added functionality worth their cost as compared to pre-shaped catheters. Pre-shaped catheters have been developed for different procedures and vessel shapes; however, IRs cannot rely on a single catheter to easily navigate through every patient’s vasculature.
Context & Scope
The purpose of this project is to create a novel base catheter that can change tip shape properties to adapt to physical changes in vasculature in real-time. The outcome of this project can improve efficiency of procedures and reduce patient blood loss, thus reducing the chances of mortality. Additionally, using fewer catheters and increasing efficiency during the procedure will reduce the overall cost of procedures.
Our design must be patentable, and therefore unique from both existing catheters and patents.
Our solution meets the needs of interventional radiologists and answers the following design question:
How might we make it easier for interventional radiologists to adapt to a patient’s unique vasculature during a procedure, in real time?
Conducting User Research
Through research, we found time and money were wasted on trying out various catheters during a procedure.
We used a mixed methods approach to understand to understand the issues with current available catheters. Our primary users are interventional radiologists. Our secondary users are radiology technologists, who are responsible for checking that a catheter is functioning correctly before handing it to the IR, in addition to tracking the catheter through imaging software to assist the IR.
✱ User Interviews: We conducted 18 1:1 semi-structured interviews with various medical professionals to uncover their experiences conducting catheter-based procedures. This included IRs, IR technologists, IR nurses, radiologists, and other surgeons. We also interviewed one senior staff R&D scientist at CR Bard, a catheter manufacturing company, to discuss the catheter market and existing designs.
✱ Fly-on-the-Wall Observations: We observed five surgical procedures and took notes on the number of catheters used, how much time was spent positioning, catheter waste, and more. This research allowed us to uncover problems with existing catheters, procedure pain points, and opportunities to improve catheter designs.
Key User Insights
IRs must use multiple catheters (3-10) to navigate patient vasculature.
1.
In cases of complex vasculature, physicians may need to use 10 times more catheters than normal.
50% of procedure time is spent orienting, rotating, and replacing catheters.
2.
Procedure cost is determined by time. We calculated that $2,550 is spent per procedure on OR costs while positioning the catheter. This includes wasted catheters that do not work or were opened but unused.
Patients experience pain during catheter repositioning and imaging fluid injection.
3.
Each catheter change or repositioning requires imaging fluid injection, which leads to more pain to the patient.
Doctors and patients are exposed to more radiation as a result of lengthy procedures.
4.
Although it’s part of the job, and doctors wear protective gear, radiation exposure can lead to diseases like cancer.
Competitive Analysis
Pre-shaped catheters come in single tip-shapes and uniform stiffnesses, which are navigated through vasculature using a guidewire. At the time of this project (2018), there were three catheters steerable in real-time on the market: The SwiftNINJA microcatheter (Merit Medical), Destino guiding sheath (Oscor), and Morph AccessPro sheath (BioCardia).
The SwiftNINJA, which of these three was most commonly used by IRs, is a microcatheter with a maneuverable tip that can be manipulated in 360 degrees to steer into small veins. The SwiftNINJA, as a microcatheter, is too small and flexible to be used as a base catheter, which this project is focused on. Further, the steerability of the catheter makes it stiffer than most other microcatheters and increases the risk of puncturing a vessel. The main reason why IRs resist using the SwiftNINJA is that it costs $2,000 per unit, which is over 40 times as expensive as pre-shaped catheters.
Design Requirements
We developed the following design requirements based on our research:
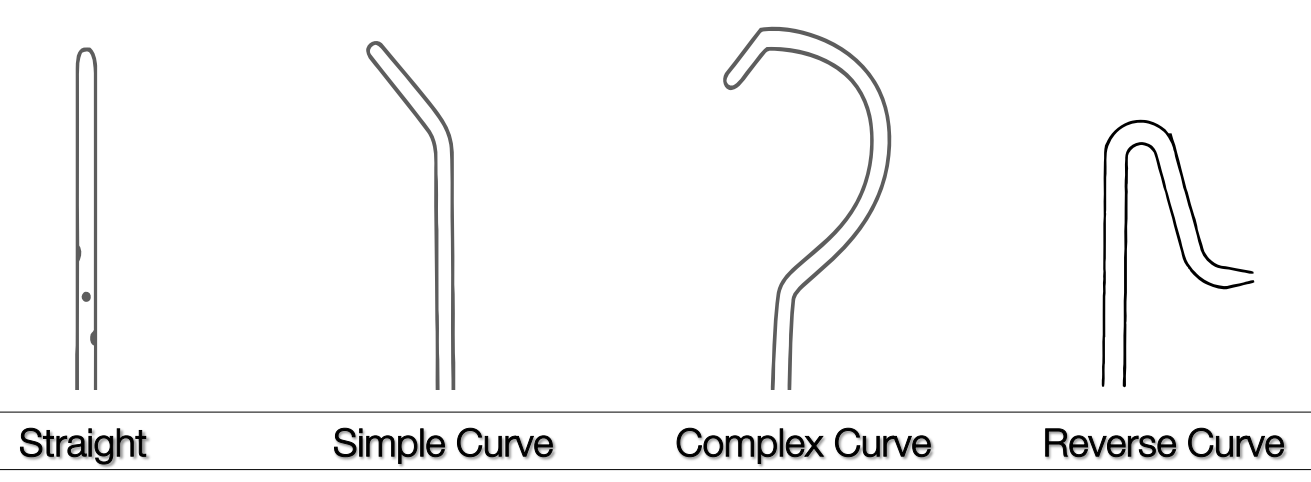
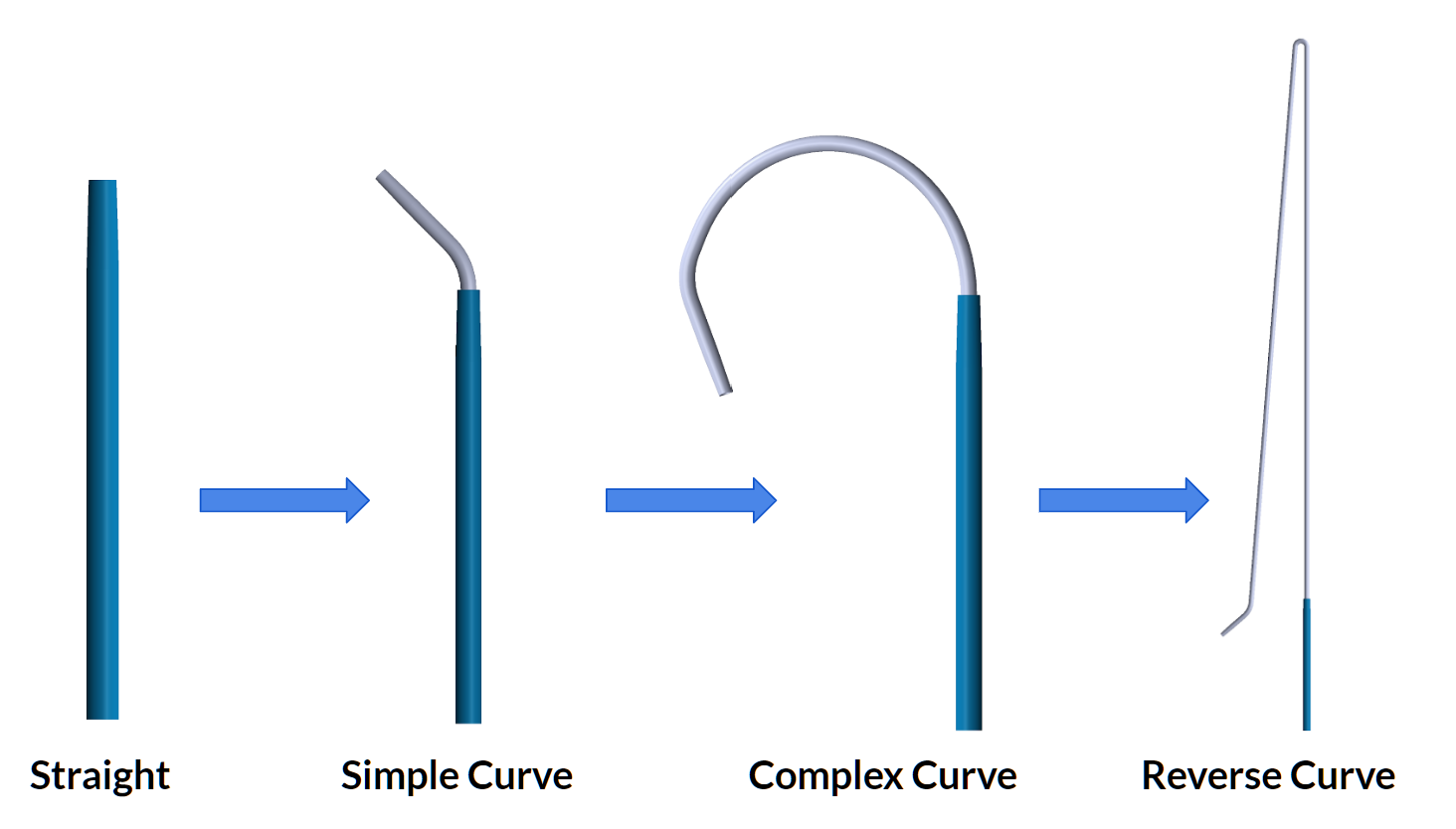
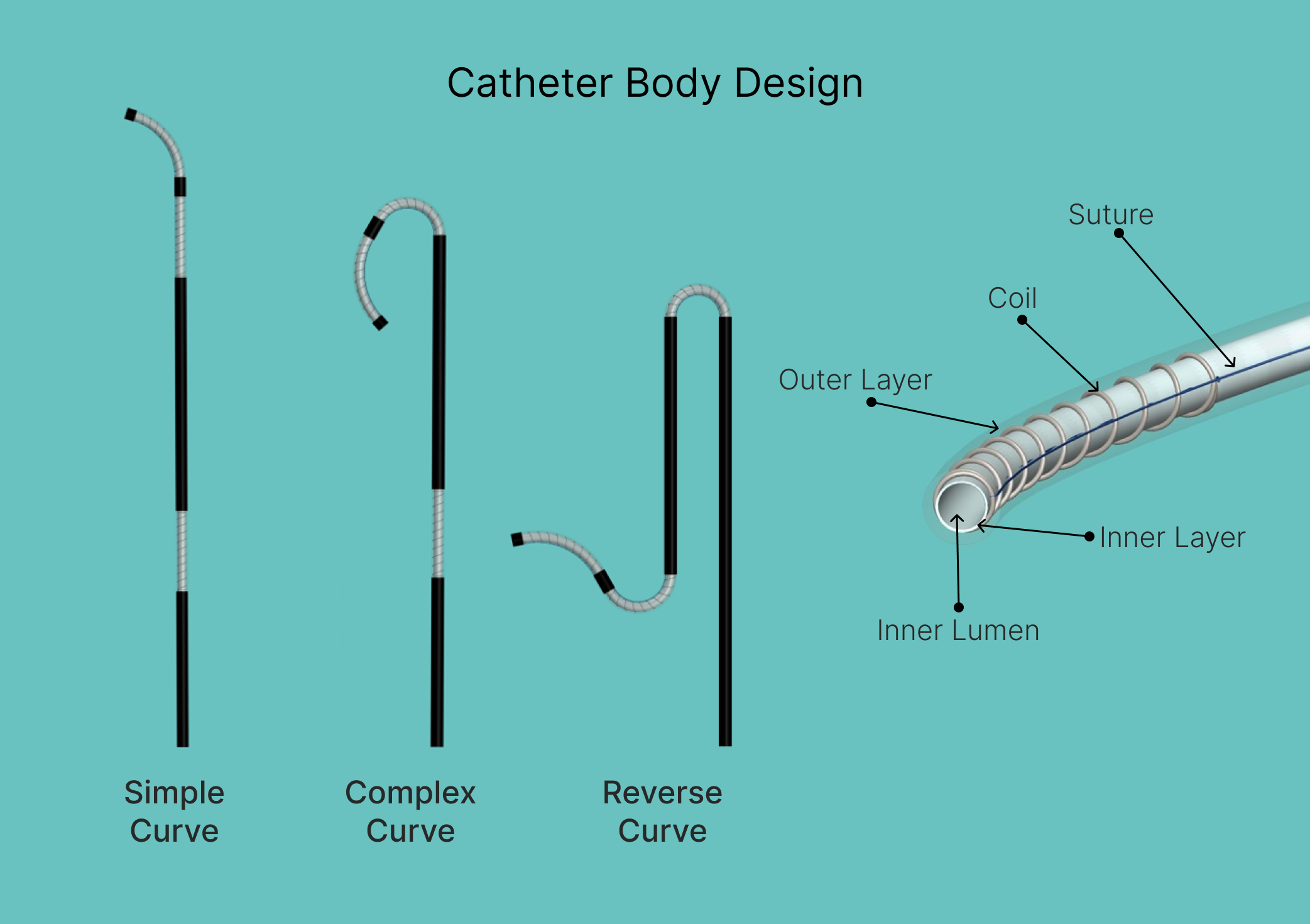
✱ Adjustable Tip Shape: The tip of the catheter can be adjusted in real-time to form the most common catheter tip shapes used: Straight, simple curve, complex curve, and reverse curve.
✱ Adjustable Stiffness: The stiffness of the catheter can be adjusted in real-time to aid in insertion and vascular navigation.
✱ Approved Materials: The catheter must be constructed with typical and regulatory-approved materials, such as polyurethane.
✱ Functions Outside of the Body: The catheter tip-shape must be manipulated through a mechanism outside of the patient’s body.
✱ Withstand Injection Fluid: The catheter must be able to withstand imaging fluid injection pressure and flow rates.
✱ Standard Dimensions: The catheter dimensions must be equivalent to standard catheters used in IR procedures.
✱ Comfortable & Easy: The catheter must be comfortable and easy to use for the user. The user must also be able to manipulate the catheter quickly with one hand.
Concept Ideation
Starting with a sketching session, we generated different ideas of catheter designs and assessed them using a decision matrix.
Prior to ideating, we conducted a thorough competitive analysis of steerable catheters and patents to ensure our device would not infringe on existing designs, as detailed above. As a team, we held a brainstorming session where we sketched ideas on sticky notes. We chose our three best designs to ideate on further.
Creating Initial Concepts
After reviewing existing catheter designs — both products on the market and patents — we sketched over 30 ideas. Below are digital sketches and 3D models of our three best concepts:
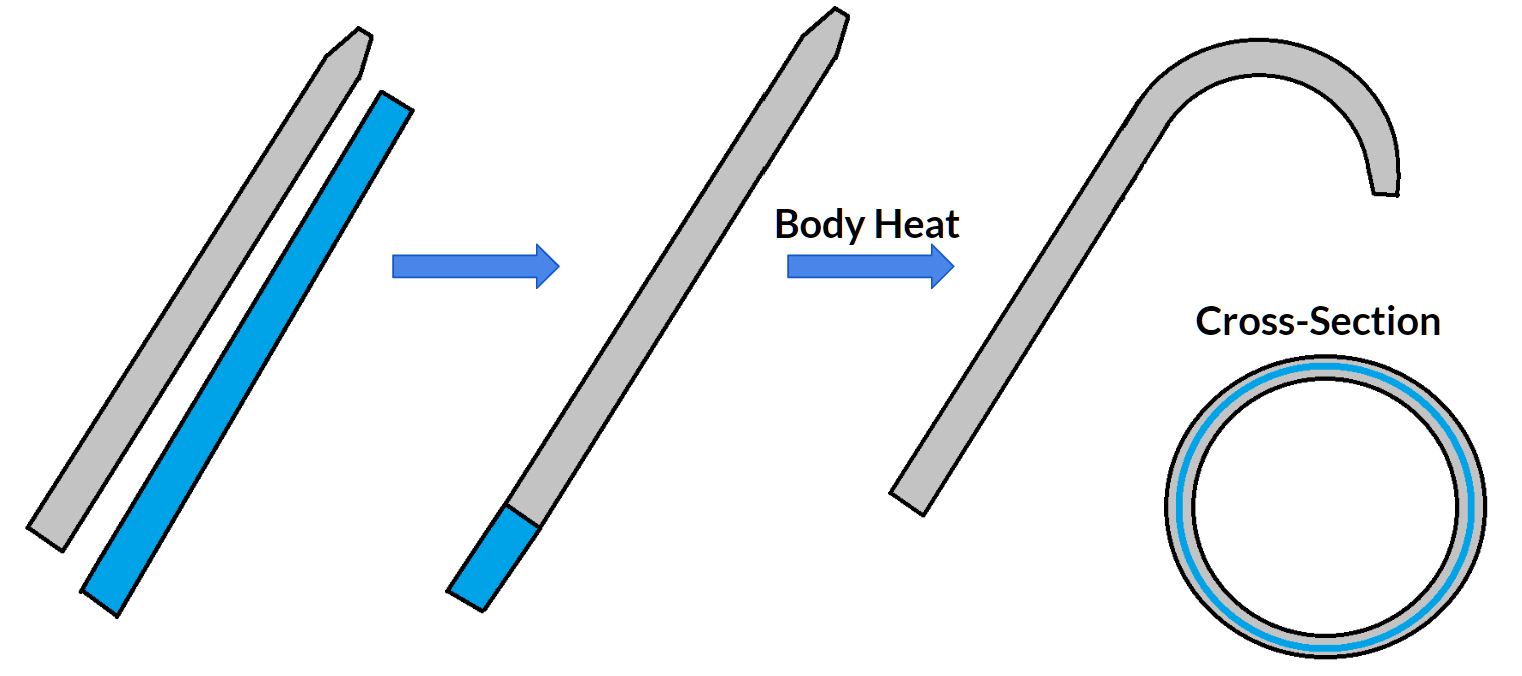
✱ Concept 1: Shape Memory Alloy
The catheter is embedded with a shape-memory alloy. When exposed to body temperature, it changes into and maintains a preset shape. However, this design only allows for a single premade shape. There would also be increased manufacturing costs and difficulties with storage and distribution.
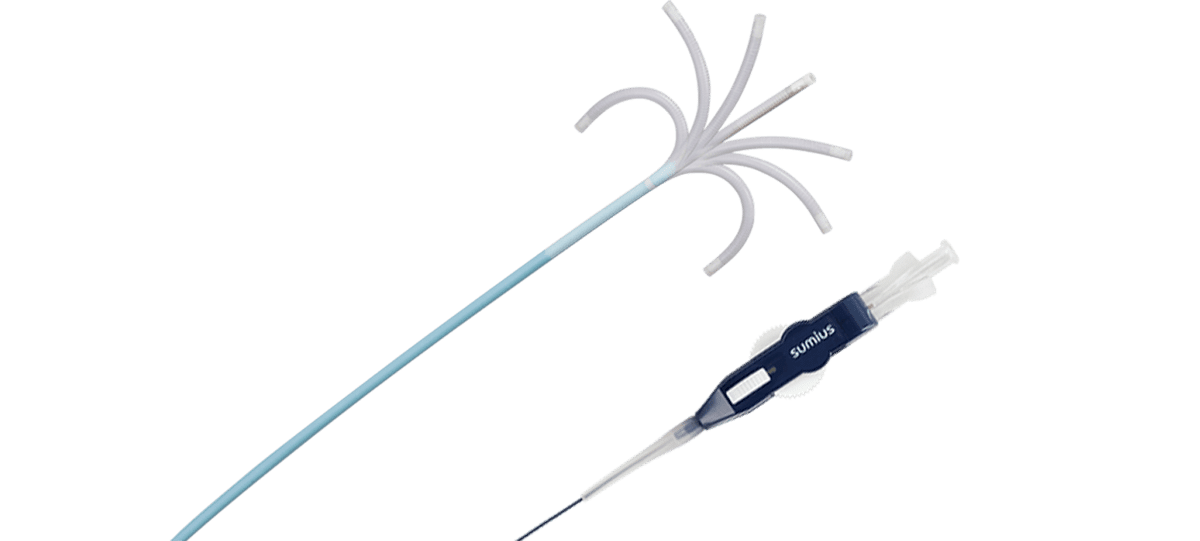
✱ Concept 2: Umbrella Sheath
This concept includes two concentric different catheters. As the inner catheter comes out of the inner catheter, it forms different shapes. Constraints of this design include a smaller lumen (inner diameter), less stiffness, and the possibility of blood clogging in areas where the inner and outer catheter meet.
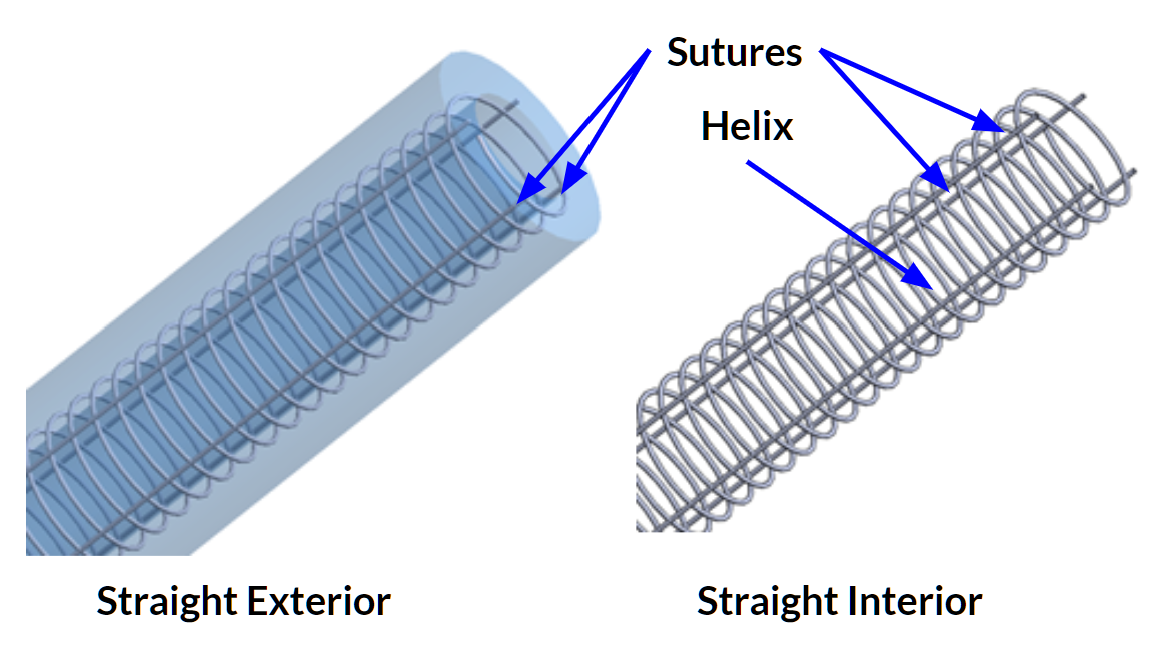
✱ Concept 3: Slinky + Suture
In this design, a coil is embedded inside of catheter walls. Sutures are attached to the coil, and run through the length of the catheter to the handle. When pulled, the coil compresses, changing the shape of the catheter. There are multiple coils located along the catheter to allow a multitude of shapes to form.
This is the design we chose to iterate on further following the results of the decision matrix, shown below.
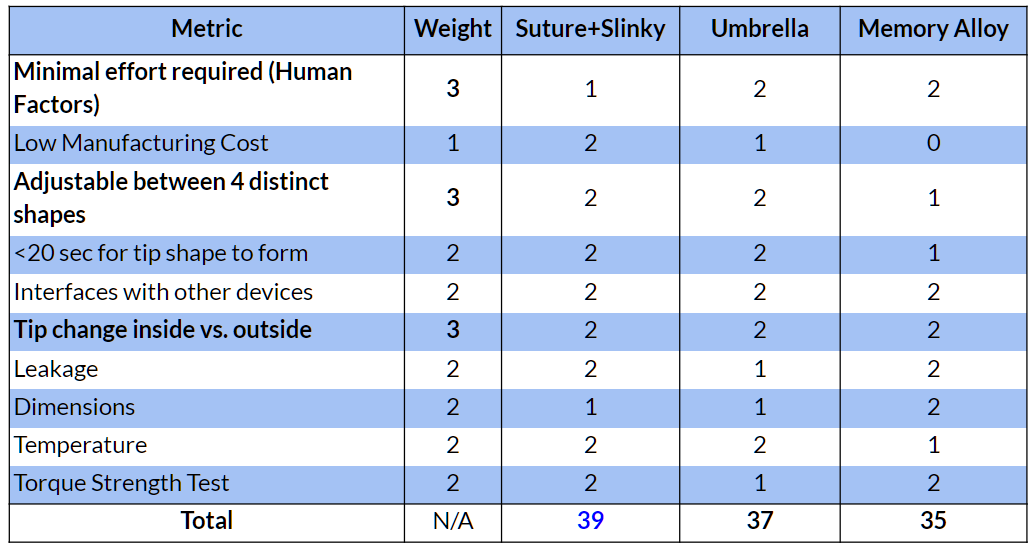
Decision Matrix
We used a weighted decision matrix with various metrics and design requirements to determine which concept to prototype further.
Following the results of the decision matrix, we began prototyping on the slinky + suture design.
Designing & Prototyping
The goal of our design solution is to provide interventional radiologists with an adaptive catheter that is more efficient and easy to use.
Design & Iteration Process
After choosing the suture + slinky concept, we began to design and prototype a functioning catheter. We started with lower fidelity materials to test out shape-changing designs, and then moved to a medium-fidelity design.
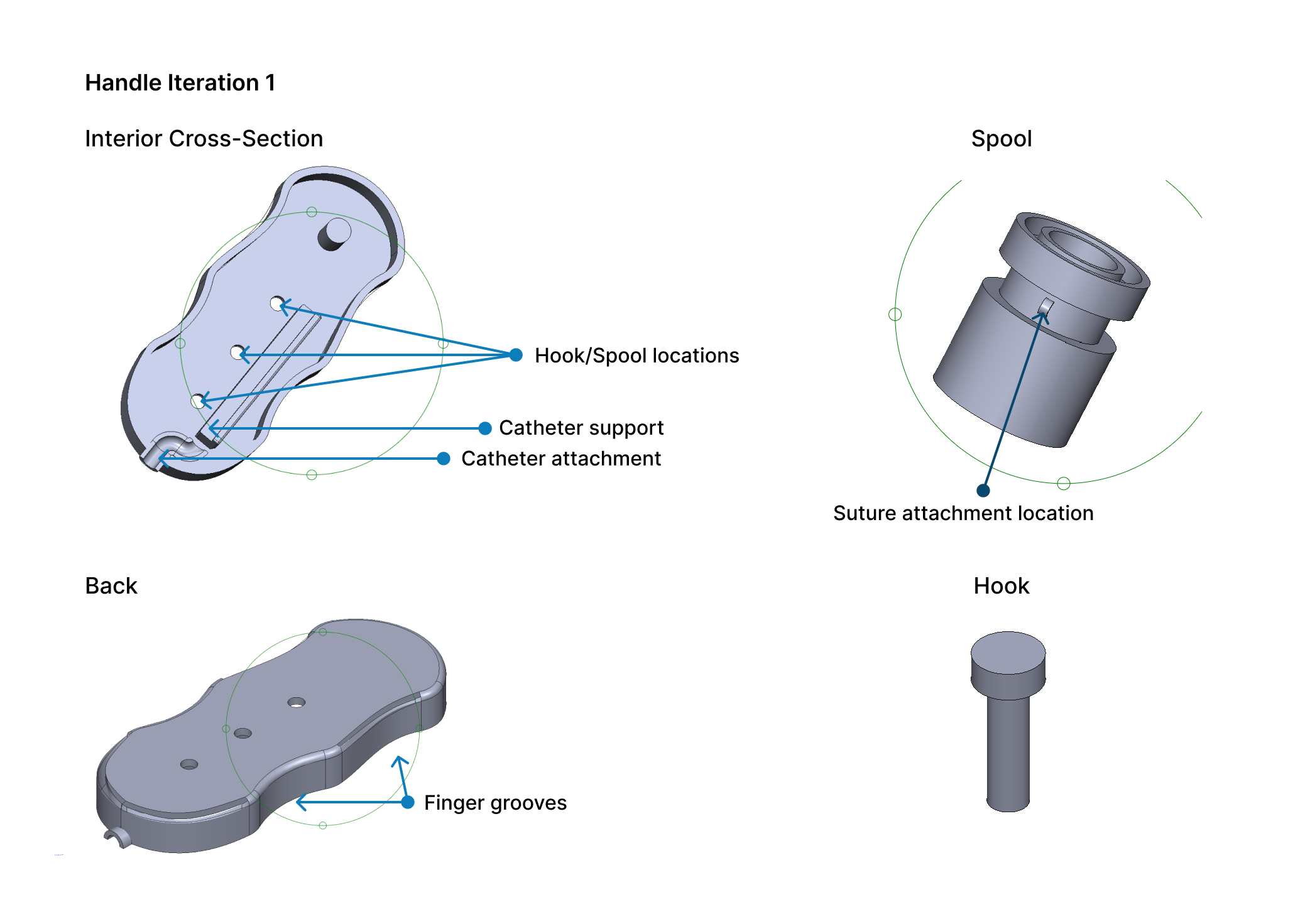
I designed the handle mechanism in SolidWorks and 3D printed prototypes. I iterated on the handle multiple times to refine the mechanism to adjust the catheter shape and to make the handle more comfortable to hold.
Prototyping Tools & Materials
SolidWorks 3D modeling software
PLA 3D priting
Polyurethane catheters
Sutures
Low- and mid-fidelity materials, including fishing line, basic coils, tape, pre-wap, etc.
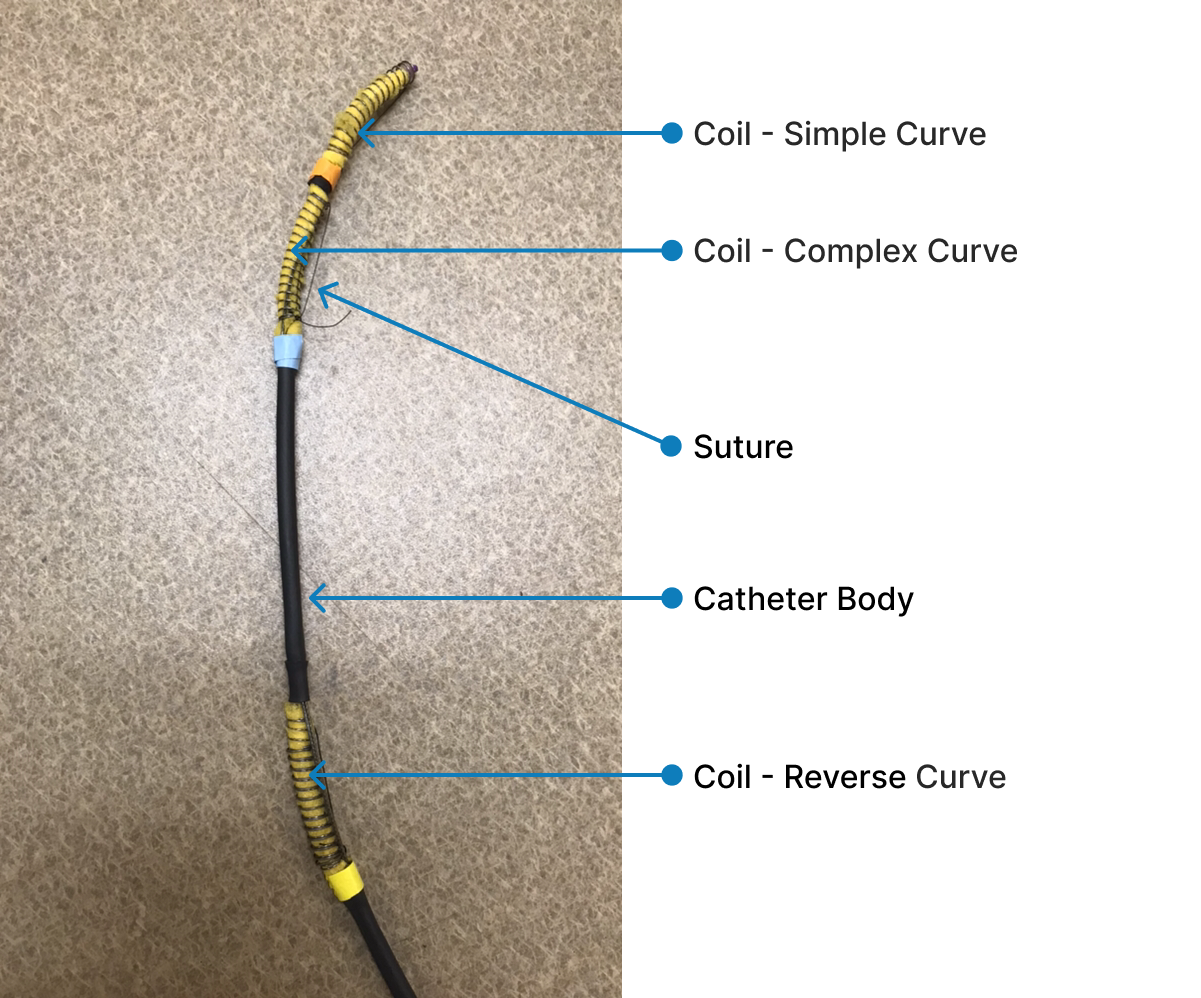
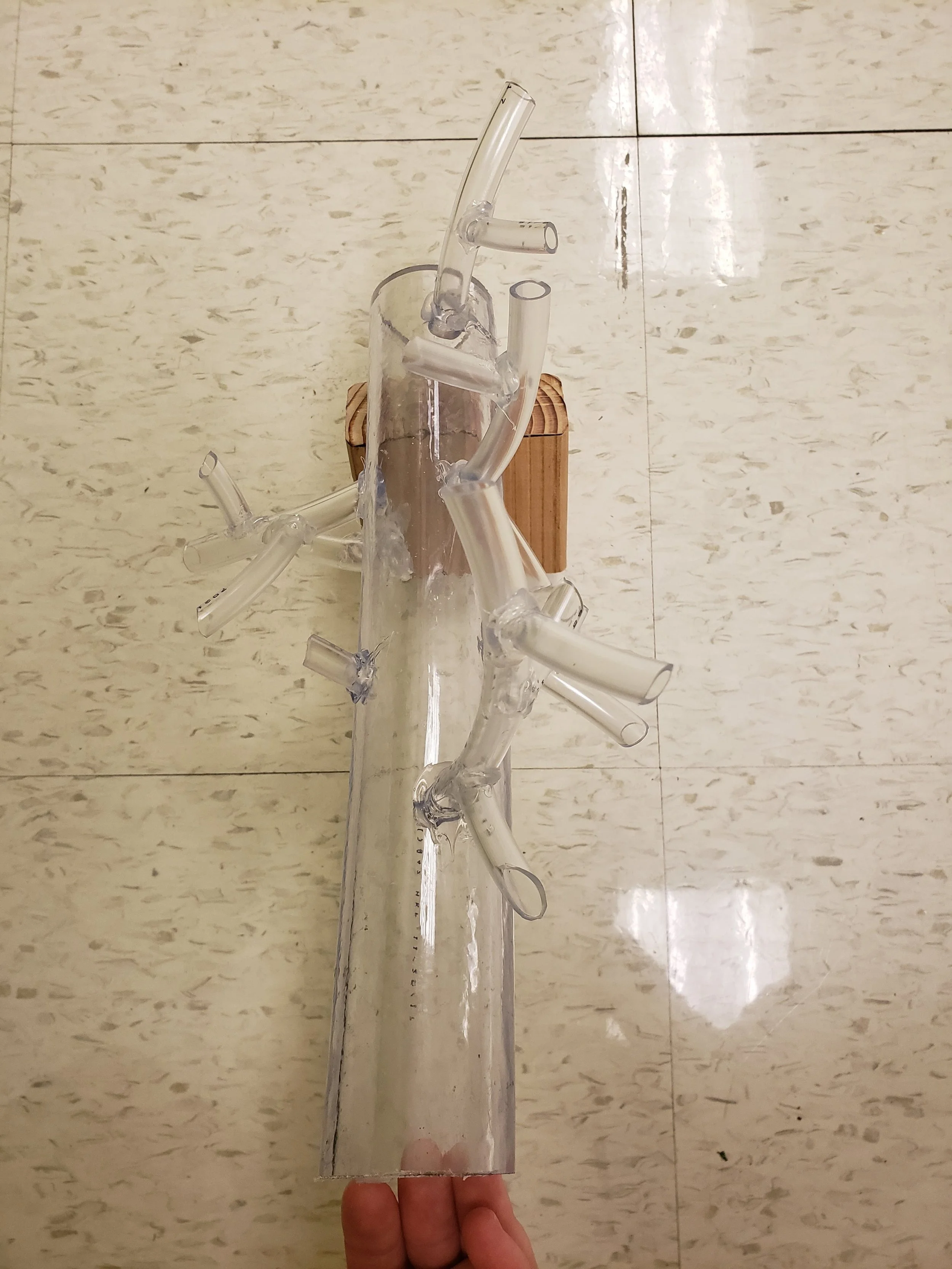
✱ Catheter Body
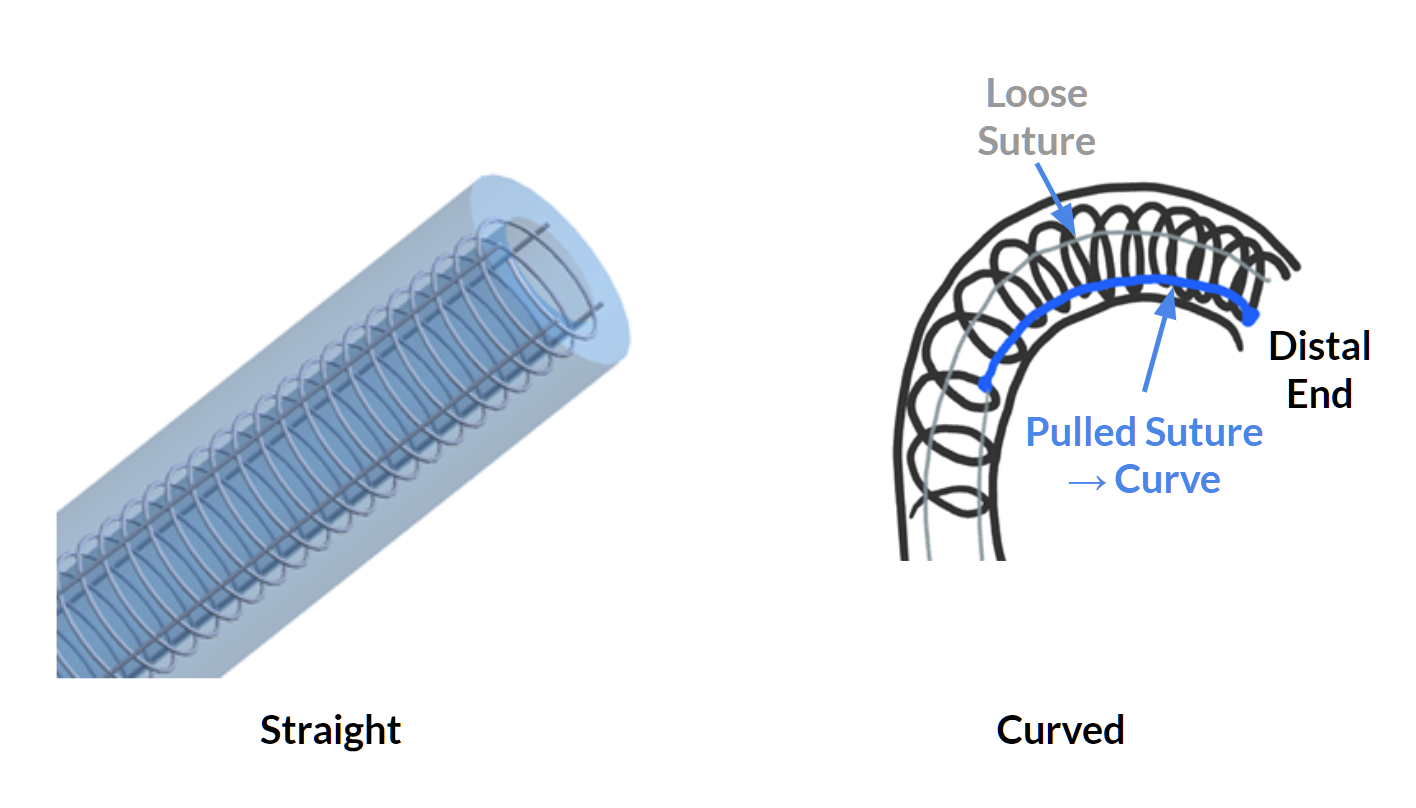
The prototype consists of a catheter with coils at three different locations along the catheter body. A suture is attached to each coil. By pulling on a suture, the catheter changes shape. The sutures are attached to the handle mechanism at the proximal end.
The prototype is made using a real catheter, real sutures, and metal coils. A thin foam-like material was used to fill the space between the coil and the catheter. Black plastic wrapping covers the areas of the catheter along the catheter body and between the coils.
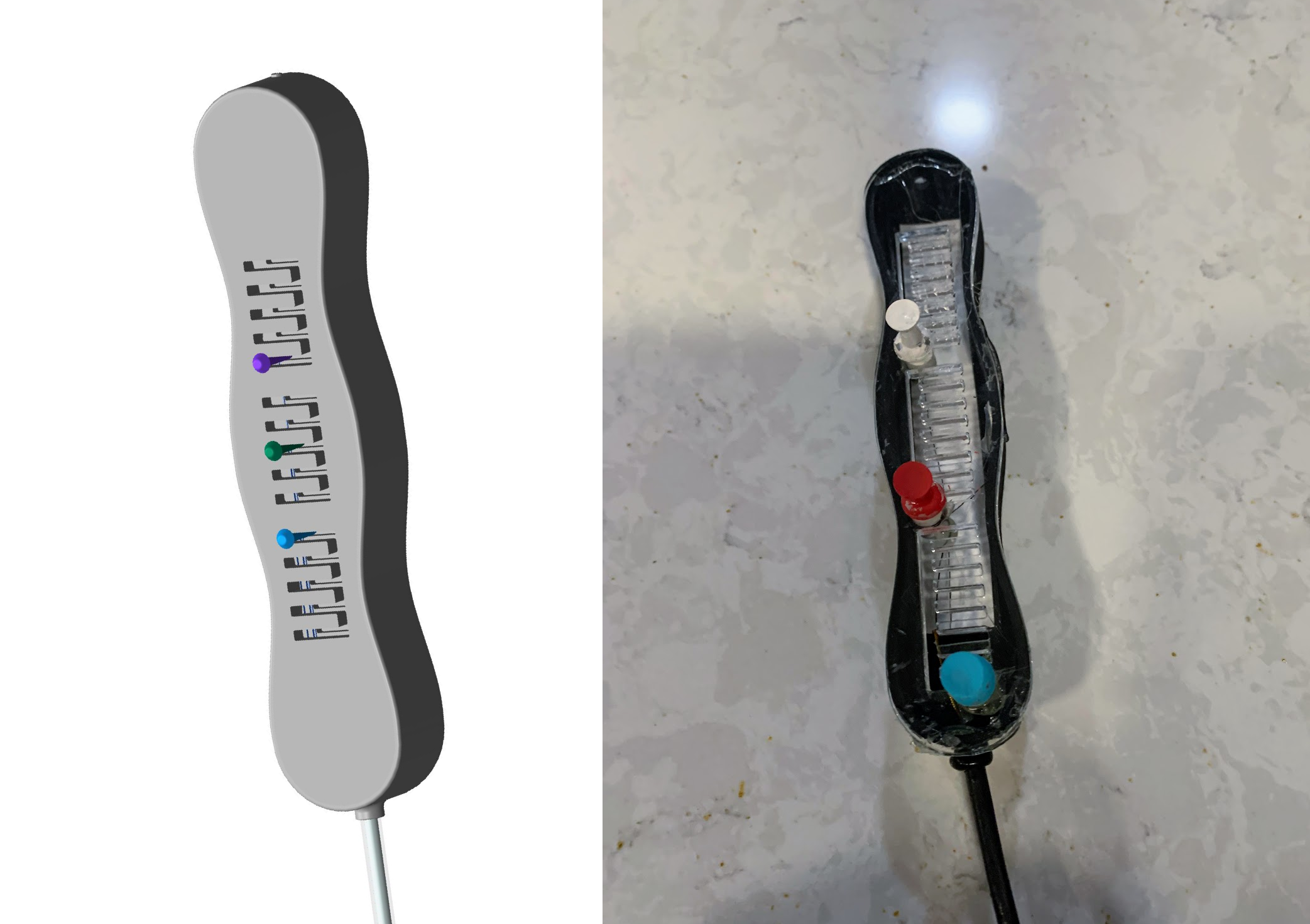
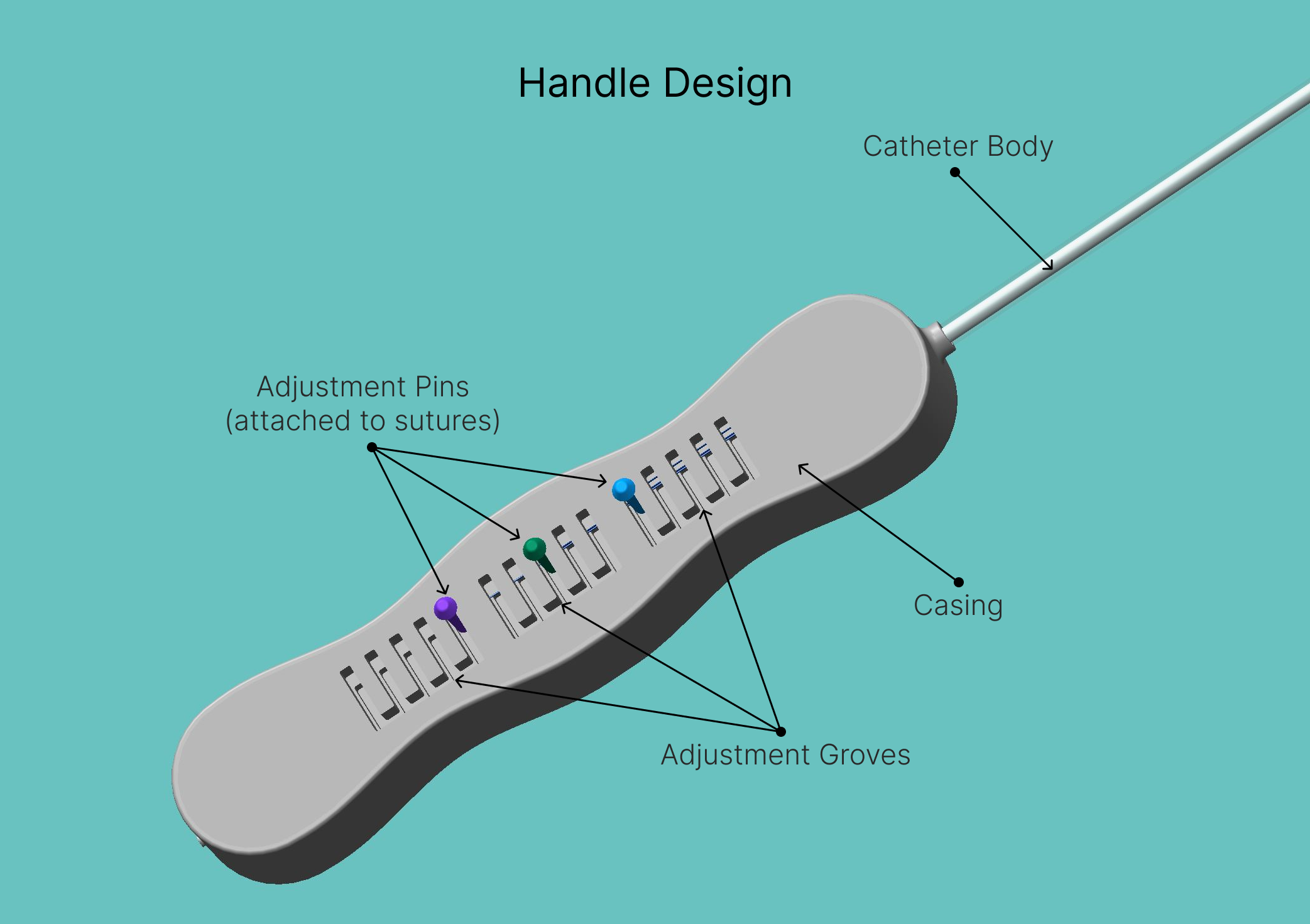
✱ Handle
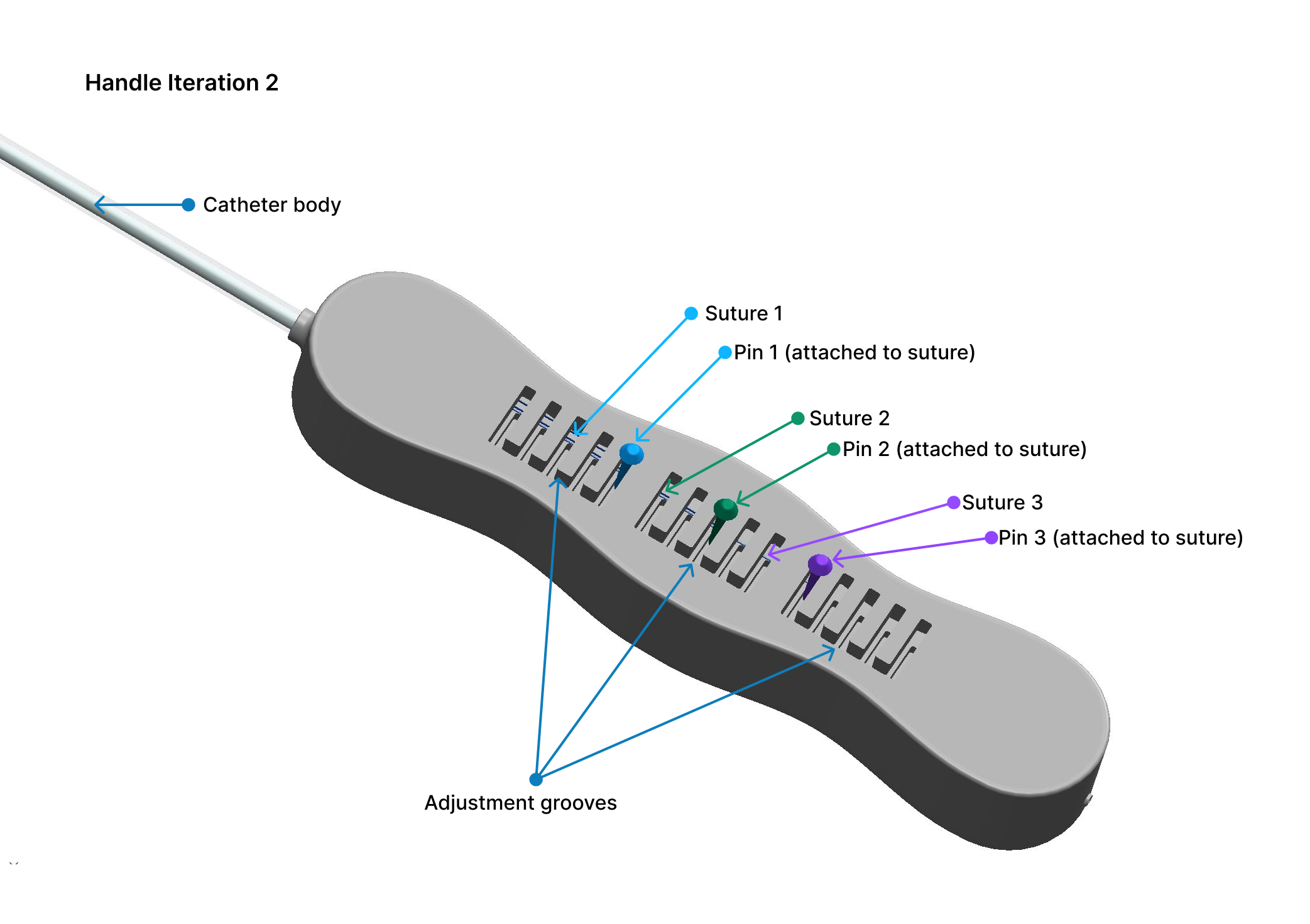
I designed the handle mechanism in SolidWorks and 3D printed prototypes. I was exploring multiple casing designs — a cross-section of an early snap fit design is pictured here. The catheter attaches inside of the casing.
I also explored different mechanisms for the suture to attach to the handle, including a hook and a spool. While I had hoped for the suture to wrap around the hook or spool as the physician adjusted the catheter tip shape, they ultimately did not work.
The next iteration of the handle mechanism involved a multi-stage adjustment. Each of the three sutures is attached to a pin, and the physician can change the position of the pin, which pulls or releases the suture, changing the shape of the coil of which the suture is attached.
Usability Testing
In the medical device world, usability testing encompasses two processes: (1) Design Validation, which is done to ensure the device is meeting user needs, and (2) Design Verification, which is done to ensure that design inputs/requirements are achieved in the final design.
Testing Goals:
Compare the prototype with existing catheters in a simulated testing environment
Assess physicians’ experience with and opinion of the prototype
Participants:
Five physicians who use intravenous catheters in their day-to-day work
Methodology:
In-person testing with five physicians, using a vasculature model. Because this was an academic project, and our prototype wasn’t made with body-safe materials, we could not test on a human or an animal. We instead built a vessel model out of plastic tubing.
Each user first attempted to access each vein branch of the model using standard catheters, and then repeated the process using our prototype.
Quantitative data collected included the time to access each vein branch, how many catheters were used, and how many vein branches were accessed
Following testing, we also administered a survey to collect qualitative data on the user’s opinions of our prototype.
Usability Findings
✱ 22% Time Saved: The user was able to access each vein 22% faster, on average, using our catheter prototype versus standard single-shape catheters.
✱ 40% More Access: The user was able to access 40% more vein branches using our catheter prototype versus standard single-shape catheters. This indicates that our design is able to access more complex vasculature.
✱ Fewer Catheters Used: Our catheter prototype is able to achieve the shapes of 10 different catheters.
Iterating the Design
Following testing, we iterated on the handle to improve comfort and suture attachments to decrease outer diameter.
Final Solution
Forme catheter is a novel arterial catheter that can change shape in real-time in response to a patient’s unique vasculature.
After usability testing, we refined our prototype. View details about our design below.
Catheter Body
The catheter body contains embedded springs at three different locations that compress to form a variety of different shapes within a single catheter.
✱ Tip Shapes
The most distal coil forms a simple curve.
The middle coil forms a complex curve.
The most proximal coil forms a reverse curve.
✱ Materials
The catheter body is made of medium-fidelity materials.
The catheter body is constructed of a polyurethane catheter.
Metal coils are attached to the polyurethane catheter, with sutures attached to each coil.
The entire length of the catheter body (outside of the coils) is covered in heat-shrink plastic.
In a real world scenario, the entire catheter body would be made of body-safe materials and would fit within the diameter constraints outlined in our design requirements.
Handle
A 3D printed handle allows the user to control the radius of each curve and lock the catheter into position where desired.
✱ Ergonomic Design
The handle is designed to fit comfortably in a physician’s hand.
The shape of the catheter can be adjusted by moving the pins. Each pin corresponds to a single coil, which is attached to a suture. When the suture is pulled or released, the coil changes shape. The pins can be pulled into one of five grooves.
✱ Materials
The catheter body is made of medium- and higfidelity materials.
The casing is made of 3D printed PLA plastic, with a laser cut acrylic top. The grooves in the top hold the pins.
The sutures are attached to pins , which themselves are attached to a foam-like material to hold them in place.
In a real world scenario, the catheter handle would be made with materials safe for an operating room.
Check out Forme in action!
A video comparing the Forme catheter prototype to single-shaped catheters using a vasculature model.
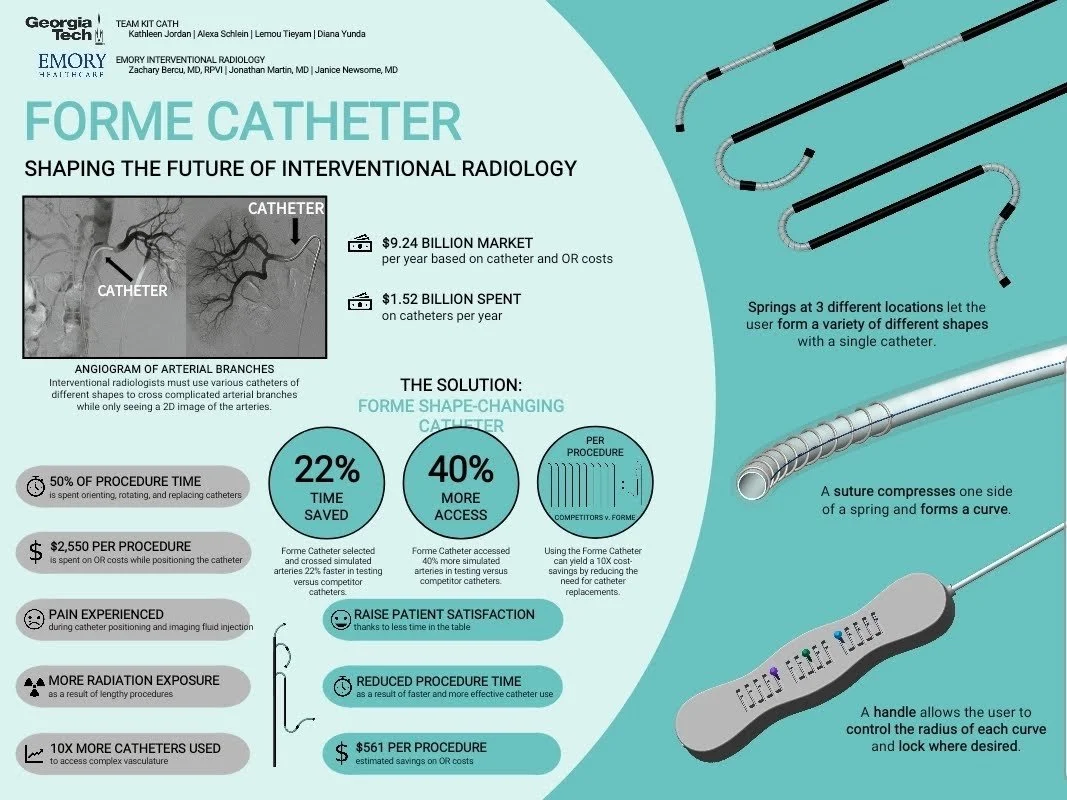
Poster
My team designed a poster to present our project. If you’d like to see a summary about the Forme project, check out the poster below or click here.
Showcase
Our project won Best Overall Project at the Spring 2018 Georgia Tech Senior Design Capstone Expo, beating out over 200 teams from various engineering disciplines. Check out an article about my team’s win!
Following the end of the semester, we also submitted our design for a provisional patent.
Key Takeaways
My biomedical engineering capstone team worked with the Interventional Radiology department at Emory University Hospital Midtown in Atlanta, GA to develop a novel catheter that can adjust tip shape in reaI-time. Inspired by a Slinky, the catheter tip can bend and adjust to the curves in a patient's vascular system, resulting in a snug fit and greatly reducing the amount of time radiologists have to spend adjusting catheters. The design reduces the number of catheter exchanges, wasted product, procedure lengths, costs, and patient discomfort.
Next Steps, Challenges, & Learnings
Future Enhancements
If I were to re-do this project, I would have wanted to explore other manufacturing techniques, such as injection molding, to test a more realistic catheter that was more accurate to our intended design. For example, an injection molded catheter could have lumens for the sutures that are intended to run along the length of the catheter.
I would also redesign the handle mechanism such that a curve can be set to any position, not just one of five groove locations.
Additionally, now with my UX training, I feel more confident in my ability to execute a design project using a standard design process that can be applied to the medical device world.
Challenges & Learnings
✱ Check dimensions carefully
The first handles I designed were far too large, and I wasted a lot of plastic in the process!
✱ Proofs of concepts don’t always prove real-world capabilities
This project was my first successful attempt at designing a medical device from scratch, from initial research through prototyping and usability testing. I learned so much about user research and designing, skills which I took into my first job out of college as a product development engineer.
Looking back, although my team did exceptionally well, our final prototype was a medium-fidelity proof of concept and was not entirely representative of a real catheter. Because this was a student project, we did not have access to the materials or manufacturing equipment used to make catheters. So, we were unable to create a prototype that fit within the majority of our design requirements (including dimensions, materials, and single-handed use) and could not be tested inside real vasculature or with imaging fluid. To this day, I’m not convinced a catheter of this design could be made without being very expensive (probably more expensive than the combined cost of single-shape catheters).
✱ Document, document, document!
I completed this project several years ago, and I unfortunately don’t have access to a lot of the images, videos, and design files. It made writing this case study quite difficult!